Simulation Best Practices
|
What is Simulation?An educational strategy designed to demonstrate procedures, decision-making
and critical thinking using devices and techniques such as role
playing to mimic clinical situations. It is an active and
collaborative style of learning. The learner has the opportunity
to share ideas, practice and skills without the stress of a real
patient. In a high risk situation it is the best method
to increase confidence and protect the patient from harm.
In a low incidence/high risk situation it may be the only way to
develop/maintain competency. |
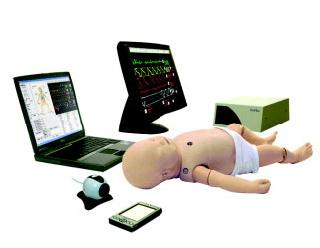
Sim Baby



Simulation Types
Partial Task Trainers
Body parts/regions with functional anatomy to practice or evaluate particular
skills.
Examples: Head/airway for intubation, Chest for Central Venous Line care
Virtual Reality
Computer simulates the physical world and the user interacts within the
world.
Examples: Adult and (soon to be) Pediatric Advanced Life Support, Disaster
training
Haptic Systems
Combines a computer-generated situation (virtual) with sensory stimuli
(partial task trainer or mannequin) to real time track competencies and
give learner feedback.
Examples: Central venous line and Peripheral intravenous line insertion
CEM (Computer-Enhanced Mannequins)
Computerized full-body mannequins that can be programmed to provide realistic
physiologic responses to practitioners actions. Used to integrate &
evaluate competencies, critical thinking, and clinical judgment. The practitioner
must synthesize knowledge, technical and communication skills and an interdisciplinary
team to manage a patient with variable complexity. Requires a realistic
environment and medical equipment/supplies.
Examples: Simulation infant, child and adult mannequins
Peer-to-Peer Learning
Collaboration used to develop and master specific skills used
to develop health and physical assessment competencies.
Examples: Listening to breath sounds, blood pressure monitoring
Standardized Patients
Case studies and role playing taught to portray and care for
patient. It is used to develop communication and critical thinking
skills.
Examples: History and assessment of a child with pneumonia
Decker,
S., Sportsman, S., Puetz, L., & Billings, L. (2008). The evolution
of simulation and its contribution to competency. The Journal
of Continuing Education in Nursing, 39 (2), 74-80.
Key Principles of Educational Practice Using Simulation
Objectives/Planning
The design and facilitating are the key components of a simulation. First,
identify objectives and be as specific as possible. Second, determine
the complexity of the skills developing or competency that will be measured.
- Determine a time frame allowing at least ¼ of the time for the debrief at the end of the session.
- Cues: Can be developed as an algorithm. If the learner performs or asks questions correctly they move in one direction. If wrong, they are asked for more information or re-direct. If the learner becomes frustrated the facilitator can re-direct with cues.
- Identify participating roles, and determine what information the learners will need prior to the simulation.
- Develop a scenario based on the target audience’s clinical environment and the simulation available to determine the best fit for their learning needs.
- Equipment failure: Finally, know your technology by troubleshooting and practicing several times before going “live”.
Facilitator Role
The skill of the facilitator is directly correlated to the quality of
the learning experience. The facilitator must aim to guide and direct
as opposed to “teach”. If there is a behavioral change that
is to occur, it may be best to create an image of “co-learner”.
- Set high expectations: be clear on time frame, objectives and ground rules. Ground rules include confidentiality, respect and any equipment stipulations.
- Support learner and empathize with the anxiety that can be provoked. Gather data to discuss within the debrief.
- Discourage competition.
- Know your target group and the practice setting. Ideally 2 people should be in any simulation. Complexity of the simulation chosen may require it-ie; CEM.
Learner Role
Set high expectations, but don’t compete. Individual needs
to be a self-directed, motivated learner. Clarify role within simulation-
can be the patient, family member, video-taper, observer-everyone should
have an identified role prior to start.
Debriefing
It is active, engaging and is structured to promote reflection. Approximately
¼ of the time allotted for the simulation is recommended to be
dedicated to the debrief.
How to debrief:
- Start with feelings. Encourage learners to express emotions related
to experience. This is an oOpportunity to regain trust, comfort and
purpose of activity.
- How do you feel about (experience)?
- How do you think it went?
- Gather feedback.
What went well?
What was challenging?
- Review the experience. Frame the learning to link to theory, content or skill. Develop a common set of experiences.
- Link to future or past experiences, events to reinforce memory and critical thinking.
- Provide a written evaluation for the simulation activity or feedback opportunity.
CHHS Simulation
- NRP
- PALS
- Mock codes
- Trauma Room course
- Competencies
- Transport team competencies
- When Seconds Count in RNO
Resources
Sites Available
- STAR lab MCW (fee charge)
- CC 4th floor CC
- 2nd floor CC
Clinicians
| Robyn Saxe | Unit-Based APN transport simulations |
| Kristin (Lewis) Braun | Trauma room simulations |
| Karen Bauer | PALS, CPR |
| Lynn Doyle | Case-based scenarios for RRT, SBARR |
| Scott Hagen MD | MCW Director of Pediatric Simulation |
| Viday Heffner MD | Emergency Medicine |
| Christina Diaz | Anesthesiology |
| Jennifer McKanry | MCW video education - CCC 4th floor |
| Cecilia Lang | Unit-Based APN mock codes |
Resources
Best Practices in Simulation Design by William Horton (PDF - March 2006)
SAEM Simulation Interest Group Simulation Scenario Template (from Robyn Saxe)
Simulation-based Application Training: A Case Study (PDF - December 2004)
Using Simulation to Enhance Medical Education (MCW site)